Detecting the early signs of deterioration in patients with confirmed or suspected COVID-19 is a significant challenge for health and social care teams. As patients at risk of poorer outcomes can be identified by reduced oxygen saturation levels, the ability to recognise early decreases in blood oxygen levels before the patient becomes symptomatic is vital.
In 2020/21, Patient Safety Collaboratives supported the successful national roll-out of pulse oximeters in their local health and care systems, both as part of the national COVID Oximetry @home and virtual ward models.
The outcomes and learning from the programme have been collated in a report, which you can download and find out more about here .
Background
The following information was compiled during the programme’s delivery in 2020/21. While Patient Safety Collaboratives are no longer directly involved in the programme, the resources below may still be useful for anyone engaged in the remote self-monitoring of oxygen saturation levels.
- COVID Oximetry @home uses pulse oximeters for patients at risk to safely self-monitor their condition at home, providing an opportunity to detect a decline in their condition that might require hospital review and admission. Early experiences of implementing this approach have been linked to reduced mortality, hospital length of stay, and the number of patients requiring intensive care admission and ventilation.
- The COVID virtual ward model is a secondary-care-led initiative to support early and safe discharge from hospital (step down care) for COVID patients. It has already been implemented in some parts of the country where it is having an impact in reducing emergency admission and builds on the COVID Oximetry @home model.
Pulse oximetry monitoring at home as part of a package of care has been recommended by the World Health Organisation.
Pulse oximetry and remote monitoring guidance has been published by NHS England and NHS Improvement along with standard operating procedures for COVID Oximetry @home and COVID virtual wards.
Read our briefing on the new COVID virtual ward model.
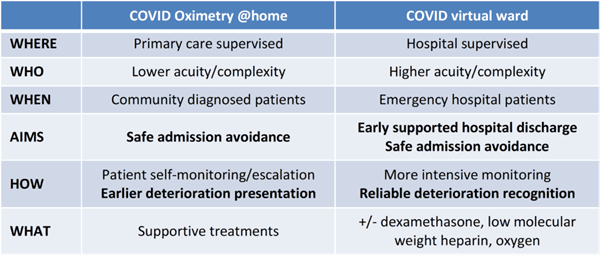
A table showing the differences between COVID Oximetry @home and COVID virtual wards (credit: Matt Inada-Kim)
What does this mean for patients?
General advice for anyone experiencing the symptoms of COVID-19 is available on the NHS website. The NHS has also published this ‘safety netting’ leaflet for people with suspected coronavirus who are isolating at home.
Patients may use a remote monitoring COVID-19 diary to track their pulse oximeter readings. Translations of the diary are available here as well as an Easy Read version.
Health Education England has produced this animation which explains how to use pulse oximeters at home and keep a COVID-19 diary:
The COVID Oximetry @home programme was featured on BBC South Today on 3 December 2020, which interviewed a Hampshire man with COVID-19, who was taken to hospital after his oxygen saturation level fell:
Learning Network
COVID Oximetry @home is part of a range of NHS at Home initiatives providing better connected, more personalised care in people’s homes, including care homes.
Resources for healthcare professionals are available in a dedicated online platform. It includes toolkits and a wealth of additional resources. These quick start guides cover how to access the COVID Oximetry @home toolkit and how to access the COVID virtual ward toolkit .
Webinars
Links are below to webinars aimed at primary care, secondary care and care homes. For a general introduction and update, watch this AHSN Network pulse oximetry session at Health Plus Care Online from 24 February 2021.
Remote monitoring using pulse oximetry in care homes
This webinar, held on 9 February 2021, is for care home staff supporting residents who are being monitored remotely using pulse oximetry. Aimed at registered managers, care workers in care homes, Primary Care Network clinical leads, and staff supporting remote monitoring, it covers why ‘silent hypoxia’ is important, how it works in practice, and the range of support and learning materials on offer.
You can download the presentation here.
COVID Oximetry @home webinar: an overview for primary care
This webinar held on 12 January 2021, highlighted the association between oxygen saturations and COVID-19 which underpins the need for the COVID Oximetry @home pathway. Hosted by the Royal College of General Practitioners and the Academic Health Science Network (AHSN Network), it shared a collaborative approach to monitor and manage patients at risk of sudden deterioration.
You can download the presentation here.
NHS England and NHS Improvement COVID virtual wards webinar: an introduction for secondary care
This webinar held on 13 January 2021 gave an overview of COVID virtual wards and the new programme. It included learning so far from virtual wards already in practice, the support that Patient Safety Collaboratives and AHSNs are offering to support implementation, and the support offer from NHSX for a digitally enabled service.
NHS England Covid Virtual Wards webinar from Wessex AHSN on Vimeo.
AHSN information
AHSNs are publishing their own case studies, resources and toolkits for local implementation of COVID Oximetry @home and virtual wards. Here are a few:
- The three South East region AHSNs (KSS, Oxford & Wessex) have published a comprehensive set of materials on the Wessex AHSN website
- Wessex AHSN has published a quick-start guide too.
- Eastern AHSN
- East Midlands AHSN
- Oxford AHSN
- West of England AHSN
This case study from Salford Royal NHS Foundation Trust describes their rapid deployment of a COVID-19 virtual ward to improve patient experience, flow and the interface to Same Day Emergency Care.
Further resources
Stop:Start simulation videos have been developed to support CCGs and trusts in setting up their COVID Oximetry @home and virtual ward services. They provide self-led training focusing on communication skills and monitoring patient safety. There are four videos and you can watch them here.
A guide on pulse oximetry for care homes has been published by the Care Provider Alliance. This document brings together existing guidance with extra detail on what this means for people who live and work in care homes.
HSJ has published this set of resources on pulse oximetry as a COVID early warning system.
Taking oximetry observations is the subject of one of the care home staff training films created by Wessex and the West of England Academic Health Science Networks (AHSNs) and West Hampshire CCG, and funded by Health Education England. This series of free videos and e-learning materials is designed to support staff working in care homes to care for residents who are at risk of deterioration. You can find more care home resources here .
This paper on Virtual Wards, Silent Hypoxia and improving COVID outcomes was published by the Royal College of General Practitioners in October 2020.
This paper on the Validation of home oxygen saturations as a marker of clinical deterioration in patients with suspected COVID-19 considers whether the early identification of deterioration in suspected COVID-19 patients managed at home enables a more timely clinical intervention.
Find out more about how AHSNs are supporting patient safety during COVID-19 and read our rapid-learning report on Safer care during COVID-19 .

“Health equity is the attainment of the highest level of health for ALL people. Achieving health equity requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and social determinants of health — and to eliminate disparities in health and health care.” (health.gov) Within the NHS there [...]

Sickle cell disease (SCD) is a serious and lifelong health condition. People with SCD produce unusually shaped red blood cells that can cause problems because they do not live as long as healthy blood cells and can block blood vessels. This can result in suffers experiencing painful episodes, called sickle cell crises, as well as anaemia, [...]

At the Royal Society of Medicine’s Tackling Inequalities conference it was clear from the passion in the room that great progress has been made across the system to better support some of our most under-served communities. To maintain this momentum, we must not just embed tackling health and healthcare inequalities in all that we do, [...]







